No 103, Caucasus Analytical Digest: Access to Healthcare
2 Jul 2018
By Gulnaz Isabekova, Nazim Habibov and Alena Auchynnika for Center for Security Studies (CSS)
The articles featured here were originally published by the Center for Security Studies (CSS) in the Caucasus Analytical Digest on 14 June 2018. external pageImagecall_made courtesy of the Official Website of the President of the Republic of Azerbaijan. external page(CC BY 4.0)call_made
Introduction by the Special Editor
Gulnaz Isabekova, University of Bremen
This issue of the Caucasus Analytical Digest focuses on access to healthcare in Armenia, Azerbaijan and Georgia. Among many factors influencing unequal access to healthcare, it discusses two major problems encountered by Armenia, Azerbaijan and Georgia in providing healthcare services. The first article by Nazim Habibov and Alena Auchynnika analyzes unequal access to healthcare services caused by unofficial under-the-table out-of-pocket payments (OOPs). It compares the level of unofficial payments in the three countries and shows their detrimental impact on patients’ access to healthcare. Based on the existing literature and empirical evidence, the authors suggest potential strategies for eliminating or reducing unofficial payments.The second article by Gulnaz Isabekova discusses unequal access to healthcare, which is caused by unequal availability of healthcare personnel. It analyzes supply, distribution and performance of healthcare workers, and their migration tendencies In the three countries. The author illustrates consequences of uneven geographic and professional distribution using the example of rural-urban, cross-country settings and concludes with policy recommendations.
Unequal Access to Healthcare and Unofficial Under-the-Table Out-of-Pocket Payments
By Nazim Habibov and Alena Auchynnika, University of Windsor
DOI: 10.3929/ethz-b-000269801
Abstract
In this study we analyse the unequal access to healthcare services in post-communist transitional Armenia, Azerbaijan, and Georgia. More specifically, we focus on how unequal access to healthcare services has caused unofficial under-the-table out-of-pocket payments. Herein, we review both the existing theoretical literature and empirical evidence on how unofficial under-the-table out-of-pocket payments lead to unequal access to healthcare services. We then analyse the precursors of paying such payments. Finally, we discuss three possible strategies to address these payments in the context of post-communist transitional countries.
Introduction
One important factor contributing to the unequal access to healthcare in post-communist transitional countries is unofficial under-the-table out-of-pocket payments (Falkingham et al., 2010; Chereches¸ et al., 2013; Stepurko et al., 2015). The payments, henceforth abbreviated as OOP, are usually defined in the healthcare research literature as monetary or in-kind contributions made by patients to healthcare personnel in exchange for services, supplies, and drugs that should formally be provided for free-of-charge (Ensor and Savelyeva, 1998; Thompson and Witter, 2000; Gaal et al., 2006a).
Unofficial Out-Of-Pocket Payments (OOP)
There are several mechanisms governing how the payment of OOPs results in unequal access to healthcare. First, OOPs are associated with a lower likelihood of using healthcare when it is needed (Balabanova et al., 2004; Falkingham, 2004; Fan and Habibov, 2009). Second, OOPs often represent catastrophically high expenditures for the poor (Habibov, 2009a, 2011). As a result, the poor are less likely to use healthcare than are the non-poor patients. Third, OOPs limit access to more advanced, up-to-date, and specialized health procedures and services; thus, the poor are forced to use less advanced procedures and services with relatively lower OOPs (Habibov, 2009b, 2010). Furthermore, OOPs lead the poor to seek consultations with less specialized healthcare personnel, and poor patients frequently must consult nurses instead of doctors.
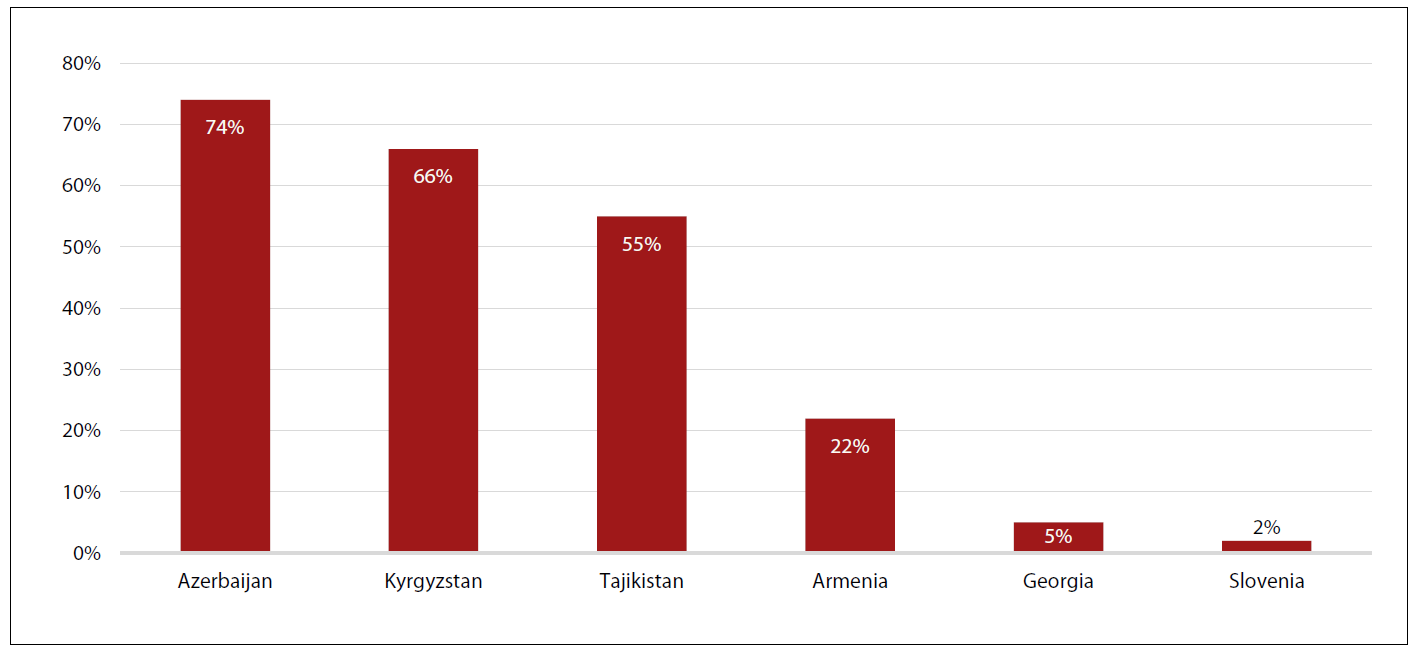
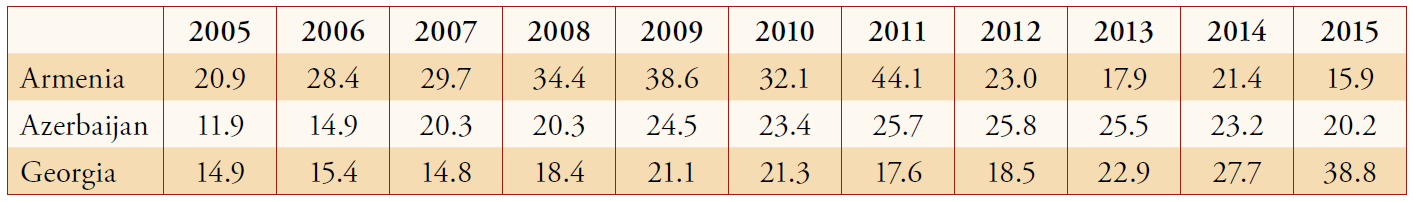
OOPs are a pervasive problem in all transitional countries, and a recent study conducted by Habibov and Cheung (2017) focused on OPPs in 29 post-communist countries of Eastern and Central Europe, the Caucasus, and Central Asia. The authors used a cross-country comparable survey and concentrated on subjects who had used healthcare during the 12 months preceding the collection of survey data. The study results showed OOPs are indeed a serious problem in the countries of the Caucasus. However, the extent of OOPs varies by country. The data indicated that approximately 74 percent of respondents who utilized healthcare in Azerbaijan had paid OOPs and that Azerbaijan had the highest rate of OOPs among all 29 post-communist countries investigated. The level of OOPs in oil-rich Azerbaijan was found to be higher than that in the less economically developed countries of Central Asia such as Kyrgyzstan, with 66 percent, and Tajikistan, with 55 percent. In comparison, the payment of OOPs in Armenia and Georgia was relatively lower at 22 percent and 5 percent, respectively. However, these levels of OOPs are still higher than those in other transitional countries, for instance, Slovenia, at 2 percent.
Explanatory Factors
The difference in OOP levels between Georgia, Armenia, and Azerbaijan can be explained by the interplay of two factors. First, the introduction of health insurance in Georgia under Mikheil Saakashvili was an important factor associated with legitimizing OOPs in the form of official insurance payments. Conversely, healthcare in Armenia and Azerbaijan follows the Semashko-model inherited from the Soviet Union that is more prone to inefficiencies, corruption, and OOPs (Gotsadze et al., 2005; Belli et al., 2004). Second, there is generally low corruption in Georgia and higher levels in Azerbaijan. Armenia is considered to have moderate levels of corruption (Habibov, 2016; Habibov and Cheung, 2016; 2017; Habibov, Cheung, and Auchynnikava, In Press).
After analysing the precursors of paying OOPs, Habibov and Cheung (2017) reported that the main determinants of OOPs included a lower quality of healthcare, as indicated by the disrespectful attitudes of healthcare personnel, lack of required drugs in healthcare facilities, frequent and unjustified absence of healthcare personnel, and longer wait times for treatment. The authors also found that individuals with poor health are more likely to pay OOPs because they utilize healthcare more often and use more advanced services such as surgery and intensive care. At the same time, Habibov and Cheung (2017) also reported that individuals from wealthier households are more likely to pay OOPs. The explanation for this phenomenon is twofold. First, wealthier people may be more willing to pay OOPs as gratitude payments since they have more resources to do so. Second, it is also plausible to assume that healthcare personnel asked wealthier patients to pay OOPs more frequently in an attempt to maximize their revenues (Belli et al., 2004; Gotsadze et al., 2005).
It is also important to note that OOP levels are not universally seen as a negative phenomenon in the context of post-communist transitional countries. The payment of OOPs is conceptualized as being a harmless cultural norm (Turex, 2011; Wang-Sheng and Guven, 2013; Bowser, 2001). In this case, OOPs are widely accepted and would not affect satisfaction with healthcare and its utilization.
Alternatively, OOPs are considered to be a positive element of development and are part of the so-called “greasing in the wheels” phenomenon (Meon and Weill, 2010). According to this conceptualization, OOPs are seen to mitigate underfunding in healthcare during the transitional period since patients expect they will need to pay OOPs to underpaid healthcare personnel for better quality services. OOPs are also considered important stimuli for competition in the healthcare sector, as patients decide to pay OOPs to get required treatment “free” through public healthcare instead of paying much higher official fees for the same treatment through private healthcare (Rose, 1998). In this case, we would expect a positive effect of OOPs on satisfaction with healthcare and its utilization. Given these different thought patterns, a recent study by Habibov (2016) evaluated the effects of OOPs on healthcare satisfaction in post-soviet nations including Armenia, Azerbaijan, and Georgia. Habibov found that a higher frequency of OOP payments in the healthcare sector undermines satisfaction with public healthcare and reduces healthcare utilization. More specifically, the elimination of OOPs would increase satisfaction with public healthcare by an average of 14 percent.
Policy Options
In the light of the available evidence, what options do the countries of the Caucasus have to eradicate, or at least reduce, OOPs? There are three main strategies. One strategy would be to legitimize informal payments by making them formal. This formalization could be done within a framework of broader healthcare reforms, but it would require a significant increase in the amount of public spending on healthcare relative to current levels (Gaal and McKee, 2004; Falkingham, 2004; Falking hamet al., 2010; WHO 2016). Another strategy would be to promote transparency and accountability in the healthcare sector. The countries of the Caucasus could join a number of existing international initiatives aimed at increasing transparency in healthcare such as the transparency initiatives funded by the Department for International Development’s (UK) Medicines Transparency Alliance or by the WHO Good Governance in Medicines Program (Vian, 2008). Finally, the last way would be to improve enforcement and clearly demonstrate that OOPs are illegal and that incidents of OOPs are considered to be corruption crimes for which perpetrators would be investigated and punished (Vian and Burak, 2006).
Figure 1: Unofficial Out-of-Pocket Payments (OOP) in Selected Countries of the Former Soviet Union and Eastern Europe (Share of Respondents Who Reported Paying OOPs)
References
- Balabanova, D., McKee, M., Pomerleau, J., Rose, R., and Haerpfer, C. (2004). Health service utilization in the former Soviet Union: evidence from eight countries. Health Service Research, 39, 1927–1950.
- Belli, P., Gotsadze, G., and Shahriari, H. (2004). Out-of-pocket and informal payments in health sector: evidence from Georgia. Health Policy, 70, 109–123.
- Bowser, D. (2001). Corruption, trust, and the danger to democratization in the former Soviet Union. In: David Lovell (Ed.), In the Transition: Essays on Post-Communism. Ashgate Publishers, London, UK, pp. 80e95.
- Chereches, R., Ungureanu, M., Sandu, P., and Rus, I. (2013). Defining informal payments in healthcare: a systematic review. Health Policy, 110, 105–114.
- Gaal, P., Belli, P., McKee, M., and Szocska, M. (2006). Informal payments for health care: definitions, distinctions, and dilemmas. Journal of Health Politics, Policy Law, 31, 251–293.
- Gaal, P., and McKee, M. (2004). Informal payment for health care and the theory of ‘‘INXIT’’. International Journal of Health Planning and Management, 19, 163–178.
- Gotsadze, G., Bennett, S., Ranson, K., and Gzirishvili, D. (2005). Health care-seeking behaviour and out-of-pocket payments in Tbilisi, Georgia. Health Policy Planning, 20, 232–242.
- Ensor, T., and Savelyeva, L. (1998). Informal payments for health care in the Former Soviet Union: some evidence from Kazakhstan. Health Policy and Planning, 13, 41–49.
- Falkingham, J. (2004). Poverty, out-of-pocket payments and access to health care: evidence from Tajikistan. Social Science and Medicine, 58, 247–258.
- Falkingham, J., Akkazieva, B., and Baschieri, A. (2010). Trends in out-of-pocket payments for health care in Kyrgyzstan, 2001–2007. Health Policy and Planning. 25, 427–436.
- Fan, L., and Habibov, N. (2009). Determinants of accessibility and affordability of health care utilization in Tajikistan in post-socialist period. Journal of Global Public Health, 4, 561–574.
- Habibov, N. (2009a). Determinants of out-of-pocket expenditures on prescribed medications in Tajikistan: Implications for healthcare sector reform. Journal of Health Organization and Management, 23, 170–182.
- Habibov, N. (2009b). What determines healthcare utilization and related out-of-pocket expenditures in Tajikistan? Lessons from a national survey. International Journal of Public Health, 54, 260–266.
- Habibov, N. (2010). Hospitalization in Tajikistan: determinants of admission, length of stay and out-of-pocket expenditures. Results of a national survey. International Journal of Health Planning and Management, 25, 251–269.
- Habibov, N. (2011). The inequity in out-of-pocket expenditures for healthcare in Tajikistan: evidence and implications from a nationally-representative survey. International Journal of Public Health, 56, 397–406.
- Habibov, N. (2016). Effect of corruption on healthcare satisfaction in post-soviet nations: A cross-country instrumental variable analysis of twelve countries. Social Science and Medicine, 152, 119–124.
- Habibov, N., & Cheung, A. (2016). The impact of unofficial out-of-pocket payments on satisfaction with education in Post-Soviet countries. International Journal of Educational Development, 49, 70–79.
- Habibov, N., and Cheung, A. (2017). Revisiting informal payments in 29 transitional countries: The scale and socio-economic correlates. Social Science & Medicine, 178, 28–37.
- Habibov, N., Cheung, A., & Auchynnikava, A. (In Press). The effects of corruption on satisfaction with local and national governments. Does corruption “grease the wheels”? Europe-Asia Studies.
- Rose, R. (1998). Getting thing done in an anti-modern society: social capital networks in Russia. Paper No. 6. World Bank, Washington, D.C.
- Stepurko, T., Pavlova, M., Gryga, I., Murauskiene, L., and Groot, W. (2015). Informal payments for health care services: the case of Lithuania, Poland and Ukraine. Journal of Eurasian Studies, 6, 46–58.
- Thompson, R., and Witter, S. (2000). Informal payments in transitional economies: implications for health sector reform. International Journal of Health Planning and Management, 15, 169–187.
- Turex, R. (2011). Corruption, attitudes, and education: survey evidence from Nepal. World Development, 39,1133–1142.
- Vian, T. (2008). Review of corruption in the health sector: theory, methods and interventions. Health Policy and Planning, 21, 392–401.
- Vian, T., and Burak, L. (2006). Beliefs about informal payments in Albania. Health Policy and Planning, 21, 392–401.
- Wang-Sheng, L., and Guven, G. (2013). Engaging in corruption: the influence of cultural values and contagion effects at the microlevel. Journal of Economic Psychology, 39, 287–300.
- WHO. (2015). Framework for addressing out-of-pocket and informal payments for health services in the Republic of Moldova. Health Policy Paper Series No. 16. WHO, Chisinau.
About the Authors
Nazim Habibov is a Professor at the University of Windsor’s School of Social Work.
Alena Auchynnika is a student at the University of Windsor’s School of Social Work.
Healthcare Workers in the Southern Caucasus: Availability, Migration and Patients’ Access to Healthcare
By Gulnaz Isabekova, University of Bremen
Abstract
The availability of qualified healthcare workers is essential to patients’ access to healthcare. An increased demand for medical workers has contributed to their shortage and uneven distribution across and within the states. Looking for a better life and career prospects, healthcare professionals move from rural to urban areas and from developing to developed countries. This article focuses on the issue of availability of medical workers in Armenia, Azerbaijan and Georgia. The analysis illustrates the unequal access to healthcare caused by the concentration of medical personnel in urban areas. Therefore, the shortage of healthcare workers is related to the uneven geographic and professional distribution, rather than to the lack of personnel. Reviewing the secondary literature on retention of medical personnel and the scarce empirical data on the three countries, this article provides policy recommendations and argues for an inclusive approach that accounts for both patients’ and medical workers’ interests.
Introduction
The increasing demand for healthcare workers has contributed to their uneven distribution within and acrossthe countries. There is a shortage of healthcare workers in the world, and it is likely to increase in the upcoming years. By 2030, the deficit of medical staff will reach 15 million, with 1.2 million in lower and upper middle-income countries in Europe and Central Asia (Liu et al., 2016, p. 9). Changing demographics, higher life expectancies and the increasing number of ageing populations are among potential contributory factors. The increased demand for healthcare professionals facilitates their migration in search for a ‘better’ life, which results in uneven distribution. There is an outflow of medical personnel from developing to developed countries, and from rural to urban areas. Uneven distribution of healthcare workers jeopardizes healthcare systems and the quality of the services. The lack of qualified personnel impacts the control of infectious diseases (Agwu and Llewelyn, 2009, p. 1665) and may result in overburdened service providers and increased diagnostic and intervention errors (Kollar and Buyx, 2013, p. 2). As a result, the populations in areas with limited number of medical personnel become more vulnerable to diseases and have limited access to quality healthcare.
This article analyses availability of healthcare workers in Armenia, Azerbaijan and Georgia and its impact on patients’ access to healthcare. Migration of medical personnel is one of the factors facilitating uneven distribution of service providers. Therefore, the first part of the article discusses this issue in the case of three countries. The following sections analyse general availability of healthcare workers by evaluating the supply or training of a sufficient number of professionals, their distribution, and performance, including the quality of their work (Liu et al., 2016, p. 2). As it is difficult to judge the performance of healthcare professionals, the paper focuses on incentives for performance and opportunities for quality improvement. By developing policy suggestions, the article argues for an inclusive approach to resolving the issue of availability of healthcare workers and their migration, which needs to account for the views of both the patients and those of medical workers.
Migration of Medical Personnel in the Southern Caucasus
In the southern Caucasus, there is considerable migration of healthcare professionals within the countries and across the post-Soviet region, while the role of migration outside the region at this stage is somewhat limited. Healthcare workers migrate for higher salaries, better working conditions and professional development opportunities. There are cases of migration to Western Europe and the United States. In Georgia, for instance, many graduates of medical universities have gone abroad, mainly to Germany or the United States, to complete their training and obtain recognized qualifications to find a job there (Lefevre and Hohmann, 2014, p. 66). There is no information on Armenia and Azerbaijan, although a similar tendency could also apply there. Joining the Bologna process, all three countries aim at improving the quality of education and the competitiveness of medical graduates, which may also contribute to their migration opportunities. But the role of migration to countries outside the former Soviet Union remains insignificant (cf. Karanikolos et al., 2014, p. 83), as the primary destination points for healthcare workers are the post-Soviet region and the Russian Federation in particular. The main reason is that along with acknowledgement of medical qualifications, migrants have almost no language barriers in Russia (Karanikolos et al., 2014, p. 83). There is no data on the number of external as well as internal healthcare migrant workers in the southern Caucasus. However, the review of secondary literature, policy documents and the Healthcare Systems in Transition (HiT) reports suggests considerable migration of healthcare professionals from rural to urban areas.
Supply of Healthcare Professionals
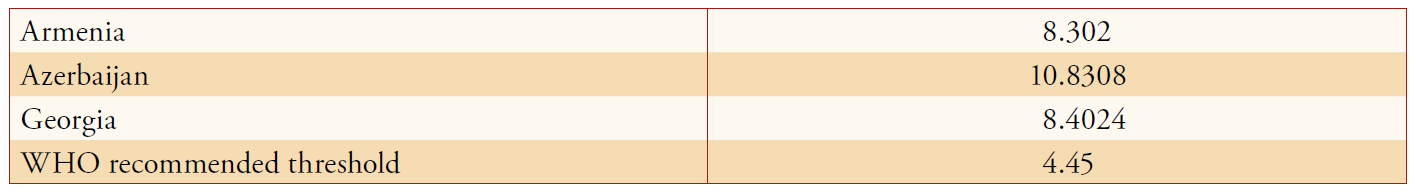
Similar to other post-Soviet countries, Armenia, Azerbaijan and Georgia train a large number of doctors. The average density of physicians as well as mid-level healthcare personnel (nurses, midwives) is much higher than the threshold of 4.45 per 1000 people recommended by the WHO (2016) (Tables 1.1 and 1.2).
There are different regulations on the supply of healthcare workers in the three states. To address the oversupply of the clinical staff in Armenia, the Ministry of Health in coordination with the Ministry of Education limits the number of state-funded positions at Yerevan State Medical University (Richardson, 2013, p. 22). This facilitates enrolment in specialties underrepresented in the market, although its impact on the reduction of overrepresented specialties is unclear. Medical education can also be obtained at private universities, outside of the state-funded positions. Similar to Armenia, the Department of Human Resources, Education and Science in the Ministry of Health of Azerbaijan analyses vacancies in the public sector and contacts medical institutions, although, since 2009, the department moved to planning according to demographic changes in the population (Ibrahimov et al., 2010, p. 57). This reflects changes from a market-driven to a needs-based approach. In contrast to both countries, Georgia seems to have no regulations on the number of graduates. The Ministry of Labour, Health and Social Affairs has limited control over the number of specialties, as it administers postgraduate education, whereas the undergraduate level is under the responsibility of the Ministry of Education (Chanturidze et al., 2009, pp. 66–67). Organization and planning of human resources is unclear. Given the large number of private universities in the country, state planning is also unlikely to work.
Undergraduate and graduate medical education in the three countries is provided by the mix of public and private institutions. After independence, the number of private institutions providing medical education increased in Georgia (Chanturidze et al., 2009, p. 62). The government did not limit their activities but introduced the unified exam for all students. The Armenian government was stricter in this regard. It refused to grant graduates of private institutions the licenses to practice medicine (Hakobyan et al., 2006, p. 97). However, there are still a number of private institutions in the country. Postgraduate training is provided by the American University of Armenia, the National Institute of Health and Yerevan State Medical University. In Azerbaijan, the government closed private medical schools by retaining the Azerbaijan Medical University as the primary institution providing undergraduate and graduate medical education.
Long after the independence Armenia, Azerbaijan and Georgia initiated reforms in medical training to comply with international standards. The states joined the Bologna process in the mid-2000s by introducing residency programmes, dividing bachelor and master studies and merging some faculties (Richardson, 2013, p. 58; Chanturidze et al., 2009, p. 67; the Ministry of Education Republic of Azerbaijan, 2009). These measures were taken to improve the quality of education and competitiveness of graduates. However, the post-Soviet region remains isolated from scientific developments in the West, such as evidence-based medicine (Karanikolos et al., 2014, p. 84), and the three countries are no exception. Medical qualifications obtained in the Southern Caucasus are primarily acknowledged in the former Soviet region, which also influences migration opportunities and preferences of the healthcare workers.
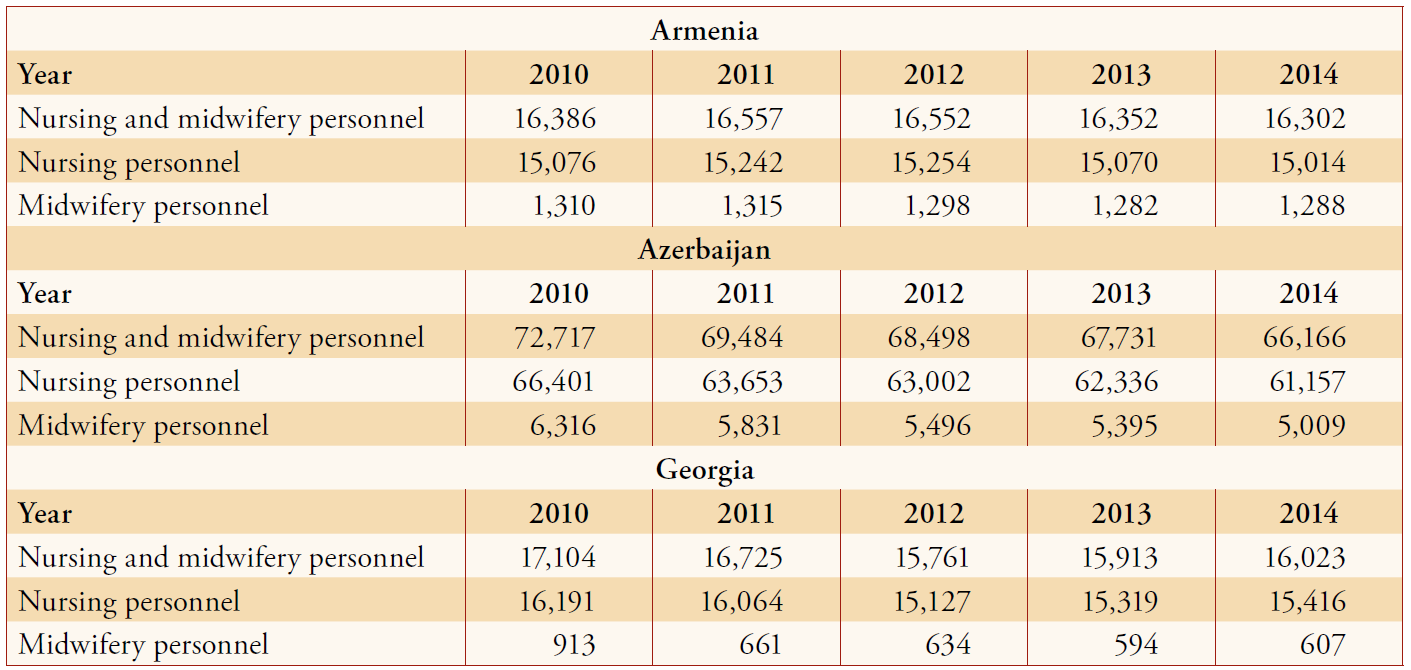
Uneven Distribution of Healthcare Workers
There is uneven distribution of healthcare workers in relation to specialties and geographic locations. This article specifically focuses on nurses and mid-level professionals. Midwives and feldshers1 provide preventive, diagnostic and therapeutic care, predominantly in rural areas (Karanikolos et al., 2014, p. 79). Therefore, their qualification is essential to patients’ access to healthcare. Armenia and Azerbaijan train two times more nurses and midwives than physicians, which complies with global dynamics (cf. World Health Organization [WHO], 2016a, p. 14). However, there is certainly an undersupply in the case of Georgia, where the ratio of physicians to nurses and midwives is almost equal (Tables 2.1 and 2.2). Underrepresentation of these professions could be related to limited educational opportunities and misperceptions among the population. Nursing, for instance, is not considered a profession (cf. Chanturidze et al., 2009). Despite differences in quantities, all three states offer limited training opportunities. In Georgia, students attend vocational school or a higher education programme to obtain the general practice or nurse title (Lahtinen et al., 2014, p.1043). In Azerbaijan, nursing is not equal to higher education, and graduates of nursing schools receive a vocational diploma (Lahtinen et al. 2014, p.1043; Ibrahimov et al., 2010, p.59). The situation is somewhat better in Armenia, where students may obtain a diploma or bachelor’s degree in nursing (Lahtinen et al., 2014, p.1043), although there are still limited opportunities for graduate education. Various international organizations and NGOs provide training courses for nurses in Armenia and Georgia (Hakobyan et al., 2006, pp. 118–119; Chanturidze et al., 2009, p. 68). However, there is no systematic approach in all three countries, and the educational opportunities for nurses as well as midwives remain limited.
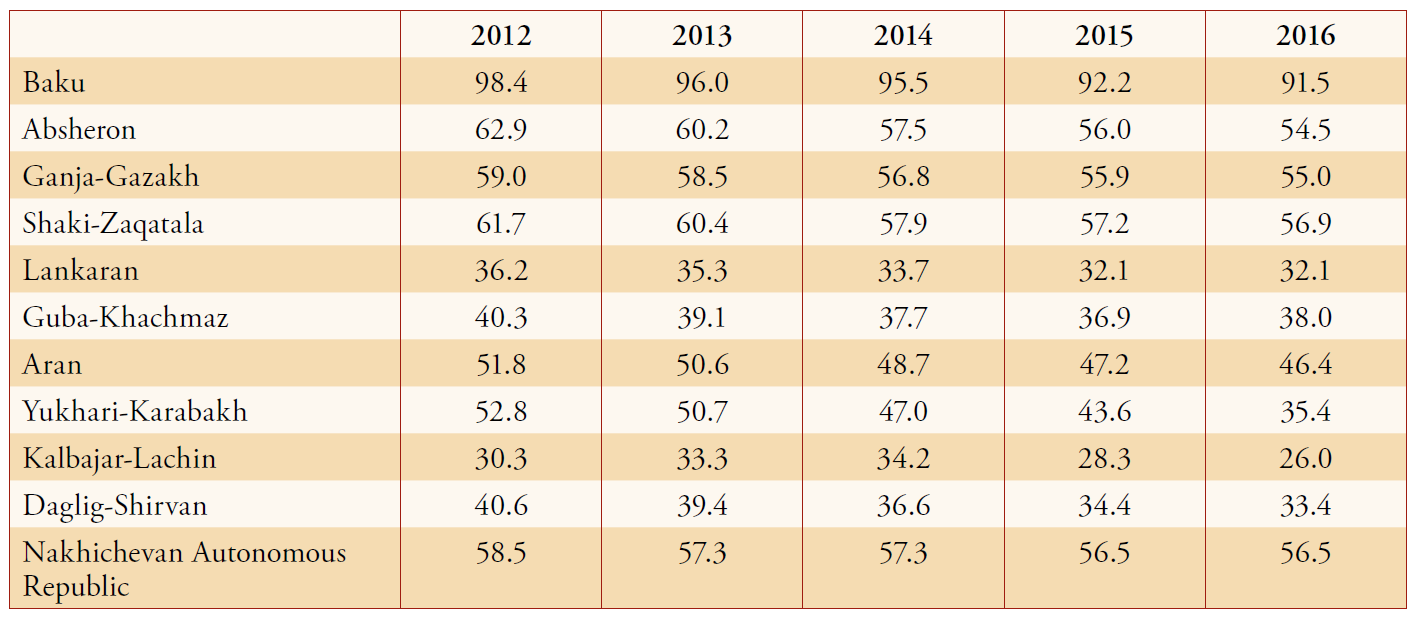
Another pressing issue in the distribution of healthcare professionals is related to geographic discrepancies. There is a considerable rural-urban inequality in the availability of healthcare professionals (Tables 3.1–3.4). Tbilisi has three times more doctors per 1000 inhabitants than any other region in Georgia, while mountainous areas suffer from the lack of specialists (Hauschild and Berkhout, 2009, pp. 22–23). Because of the decreasing population in certain rural areas, village doctors in Armenia are not replaced, and following the staff rationalization programme, an emphasis was placed on urban healthcare centres and hospitals (Lefevre and Hohmann 2014, p. 57). 70% of physicians, 63% of hospital beds and 29% of ambulatory and polyclinic facilities are concentrated in Yerevan (National Statistical Service of the Republic of Armenia and the World Bank 2017, p. 130). In Azerbaijan, 30% of positions for paediatricians and gynaecologists remain vacant in rural areas, with similar positions in urban areas being overcrowded (Ibrahimov et al., 2010, p. 100). A large and dense concentration of healthcare professionals and facilities in large cities, or mainly capitals, in all three countries suggests significant inequality in accessing healthcare.
The unequal distribution of healthcare professionals influences access to services and their quality. The concentration of the staff in urban areas limits the number of services in rural healthcare facilities. The unavailability of obstetric care (care during and after pregnancy) in Armenia contributes to the rural-urban divide (WHO Regional Office for Europe, 2010, p. 11). Looking for services, patients refer to city hospitals or search for other local alternatives. Hence, the issue of institutional delivery in rural and disadvantaged areas of Azerbaijan is resolved by assistance and birth attendance for deliveries at home (Joseph et al., 2016, pp. 6–11). There is a decline in personnel and skills in rural areas, and the staff members without support often make critical decisions (Balabanova and Coker, 2008, p. 632). Healthcare personnel might also be overburdened if the positions of colleagues remain vacant. This influences the referral tendencies among the population. As the rural feldsher ambulatory stations are understaffed, patients in Azerbaijan prefer to directly refer to district hospitals (Rzayeva, 2013, pp. 49–50). This tendency may further contribute to the deterioration of local facilities and the concentration of professionals in urban areas. However, referral to city hospitals is not affordable to all, as it incurs transportation and accommodation, in addition to service costs. Therefore, the uneven distribution of healthcare professionals in rural areas creates inequity in accessing the healthcare services.
Incentives for Improving Performance and Quality of Work
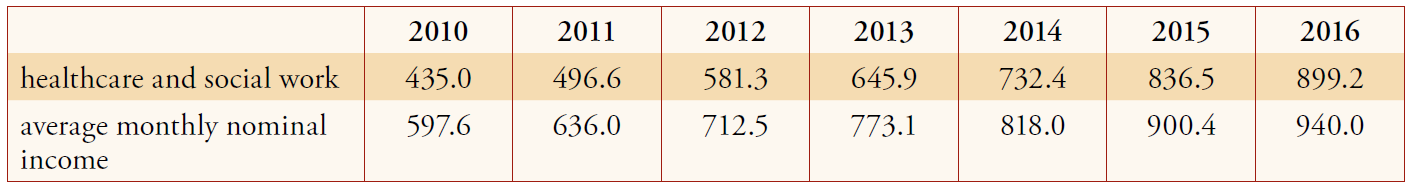
As there is limited information on the quality of healthcare services in post-Soviet countries (meaning that there is no indicator to compare across the countries), this section of the article will focus on incentives provided to healthcare professionals, such as salary (as well as bonus payments) and continuing education. The three countries have comparatively low spending on healthcare in comparison to other countries in the post-Soviet region, and the share of general government health expenditure is also small (Tables 4.1 and 4.2 on p. 16). The nominal salaries are above the minimum wage level, defined by the law, but nevertheless remain low (Tables 5.1–5.3).
Countries have different regulations and mechanisms for paying the healthcare workers. The healthcare workers in Armenia are contracted since the country’s independence. The number of staff and remuneration is defined by hospital directors (Richardson, 2013, p. 54; Hovhannisyan et al., 2001, p. 58). The government intervenes only in cases of healthcare workers providing state-financed services, such as primary healthcare (Hakobyan et al., 2006, p. 60). In this case, the state pays healthcare facilities according to the number of people enrolled and makes bonus payments for achieving the healthcare indicators (Petrosyan et al., 2017). In this situation, healthcare providers are incentivized to improve the quality of services to retain patients and improve outcomes to meet target indicators. Similar to Armenia, the healthcare staff in Georgia is contracted by health facilities. The managers of healthcare facilities define salaries and there is a growing interest in increasing payments to keep qualified personnel (Chanturidze et al., 2009, p. 48). However, the general level of wages remains low. The government provides higher payment rates for physicians working in remote areas to incentivize them (Gamkrelidze et al., 2002, p. 59). It also encouraged the independence of rural PHC doctors by changing their status. Previously employed by a district polyclinic, they became budget holders, deciding their own payment by economizing in other areas (Chanturidze et al., 2009, p. 48). In other words, they gained the capacity to allocate available budget to increase remuneration. In contrast to the other two countries, Azerbaijan retained centralized control over the healthcare providers. Salaries are defined according to the unified tariff scale, with co-payments for working with certain diseases (Ibrahimov et al., 2010, pp. 38–39). However, the average salary for healthcare personnel is below the average for other professions, and additional benefits, such as free housing and utilities, available under the former Soviet Union, have been abolished (Rzayeva, 2013, p. 46). In general, all three countries have low salaries. Therefore, healthcare workers are incentivized to ask patients for informal payments (Richardson, 2013, pp. 46–47; Holley et al., 2004, 52; Gamkrelidze et al., 2002, p.50). Without increasing wages, the situation with ’under the table’ payments are likely to remain despite the reforms on officialising them.
In addition to financial benefits, professional development opportunities, such as continuing medical education, contribute to service quality improvements and incentivize the staff to perform better. The countries vary in terms of the available options. Continuing medical education courses are provided by medical institutions
or international organizations operating in these countries. All physicians and nurses in Azerbaijan are required to pass a certification every five years, including a written test and an interview (Karanikolos et al., 2014, p. 88). Armenia has similar relicensing terms with additional requirements for continuing medical education
and professional development (Richardson, 2013, p. 59; Hovhannisyan et al., 2001, p. 58). The country recently introduced the credit model (News.am, 2017). The government demands that healthcare professionals take additional courses to improve their qualification. In contrast to Armenia, there is no requirement for continuing medical education in Georgia. It is desirable or voluntary, but not mandatory (Chakhava and Kandelaki, 2013, p. 21). At the same time, the self-financing requirement for these courses (cf. Karanikolos et al., 2014, p. 88) could be problematic, as their accessibility to medical personnel with low salaries, such as physicians and nurses, could be challenging.
Policy Suggestions
Based on the analysis of the supply of healthcare professionals, their distribution, performance incentives and opportunities for continued education, the following policy suggestions could be generated:
First, there is a need for a comprehensive human resource planning policy addressing the needs of the population and healthcare workers. Labour dynamics or needs-based approaches are unlikely to work without considering the interests of service providers. This may result in unemployment of healthcare professionals along with unfilled vacancies (McPake et al., 2013, p. 841; Liu et al., 2016, pp. 2–3). Although there is no information on the number of healthcare workers unemployed in the three countries, there is certainly a mismatch between the large number of graduates and vacant positions in rural areas. The failure to account for healthcare workers’ preferences could be the key in understanding this situation. The mandatory assignment of medical graduates to regional facilities, as suggested in the case of Azerbaijan, is unlikely to work without additional incentives. The healthcare workers will possibly use informal connections to find a job elsewhere (McPake et al., 2013, p. 841). The potential incentives could include a faster promotion track, training, fellowships and grants for healthcare personnel from rural areas (Kollar and Buyx, 2013, p. 6). This may also include financial rewards, such as additional bonuses to the salary. All these measures might be demanding for the state budget. However, given a targeted implementation with the focus on certain regions or specialities (Araujo and Dussault, 2017a, p. 385), incentives might be feasible. They could facilitate attracting more graduates to remote areas, although their retention there is unlikely.
Second, regional inequity in accessing healthcare could be targeted by training mid-level professionals and mobilizing local communities. The internal and external migration of the healthcare workers is inevitable. One of the solutions is to strengthen training and increase the number of mid-level professionals. Focussing on them, rather than doctors, may ensure access to basic services (Ghimire et al., 2009, p. 291). This will require reforms in medical education, providing more opportunities for nurses and midwives to obtain undergraduate and graduate education. This could be combined with residency programmes in rural health facilities. An acknowledgement of the importance of mid-level healthcare personnel will also contribute to changing the perception of their importance and value to the healthcare system. Furthermore, local community representatives could be trained to assist them. Community representatives could serve basic healthcare needs to ensure the access to preventive care in remote areas (Nair and Webster, 2013, p. 160). This may include, for instance, awareness-raising about infectious diseases, hygiene, sanitation and promoting a healthy lifestyle.
Third, there is an acute need for providing incentives to healthcare workers by increasing the salaries and improving the access to continuing medical education. Higher wages could contribute to retention of healthcare workers. Certainly, migration of healthcare workers, both internal and external, is driven by a number of factors. This may refer to a better lifestyle, opportunities, education for their children and safer working conditions (Ghimire et al., 2009, p. 291). All these factors cannot be targeted in the reform programme, as they are related to a broader socioeconomic and political situation beyond the healthcare system. However, targeted actions could be taken to address the essentials, such as salaries and professional development. Empirical studies show little except the impact of wage changes on the supply of doctors and nurses (Araujo and Dussault, 2017b, pp. 383–384). Extremely low wages facilitate informal payments, ‘brain drain’ of healthcare professionals in search for a ‘better life.’ A substantial increase in salaries is unlikely given the economic situation in these three states (although paradoxical in the case of Azerbaijan). Therefore, a feasible wage increase needs to be complemented with other incentives. This may include safer working conditions, continuous training and reward for performance (Araujo and Dussault, 2017a, p. 385). Particular importance can be given to opportunities for professional development and better living and working conditions, as these measures are known to be more efficient than higher wages (Nair and Webster 2013, p. 160). One of the first steps could be providing opportunities for continuous medical education. As self-financing for these courses is challenging, the government could collaborate with international organizations and international professional associations to support and subsidize the costs, or offer the courses as rewards for working in regions and remote areas. A combined implementation of all these measures could facilitate better performance and quality improvements.
Conclusion
Following a global trend, there is a shortage of healthcare professionals in three countries in the southern Caucasus, although this shortage is mainly related to an uneven distribution across the professions and geographic locations rather than an insufficient supply. Similar to other countries with low healthcare spending, the three states are vulnerable to an outflow of qualified staff to the Russian Federation or beyond. However, the analysis also shows that there is considerable internal migration of healthcare professionals that causes unequal access to healthcare within the countries. Armenia, Azerbaijan and Georgia have different state regulations on the supply of medical graduates, salaries and incentives for healthcare professionals. However, the countries share a number of commonalities, such as low wages, an oversupply of doctors, an undersupply of mid-level workers and limited opportunities for professional development. To target these issues, the countries need to develop an inclusive policy for human resources planning, which should take into account the interests of both patients and service providers. Otherwise, the phenomenon of a large number of graduates with medical education and unemployment together with unfilled positions in these countries is likely to remain.
Notes
1 Healthcare workers providing basic medical care, mostly in rural areas.
References
- Agwu, K. and Llewelyn, M. (2009). On behalf of undergraduates in International Health at UCL: Compensation for the brain drain from developing countries. The Lancet, 373, pp. 1665–1666.
- Araujo, E.C. and Dussault, G. (2017). Dynamics of the Health-Care Labor Markets. In: S. R. Quah, W.C. Cockerham, ed., International Encyclopedia of Public Health, 2nd ed. Volume 2. Oxford: Academic Press, pp. 382–386.
- Balabanova, D. and Coker, R. (2008), Russia and Former USSR, Health Systems of. In: K. Heggenhougen, S.R.
- Quah, ed., International encyclopedia of public health. Amsterdam, Boston: Elsevier/Academic Press, pp. 627 637.
- Chakhava, G. and Kandelaki, N. (2013). Overview of legal aspects of Continuing Medical Education/Continuing
Professional Development in Georgia. Journal of European Continuing Medical Education, 2(1), pp. 19–23. - Chanturidze, T., Ugulava, T., Durán, A., Ensor, T., Richardson, E. (2009). Georgia. Health system review. Health Systems in Transition, 11 (8). 1–114.
- Gamkrelidze, A., Atun, R., Gotsadze, G., MacLehose, L., McKee, M. (2002). Health Care Systems in Transition. Georgia. Health Care Systems in Transition, 4 (2), pp. 1–72.
- Ghimire, L. V., Malekpour, M., Fatehizadeh, M., Hashemian, R., Mohammad, S., Velayati, A.A. (2009). Retaining health manpower in developing countries. The Lancet, 374, p. 291.
- Hakobyan, T., Nazaretyan, M., Makarova, T., Aristakesyan, M., Margaryants, H., Nolte, E. (2006). Armenia. Health system review. Health Systems in Transition, 8(6), pp. 1–180.
- Hauschild, T. and Berkhout, E. (2009). Health-Care Reform in Georgia. A Civil-Society Perspective: Country Case Study. Oxfam research report, [online], pp. 1–47. Available online at <https://www.oxfam.org/sites/www.oxfam. org/files/healthcare-reform-georgia-report-0905.pdf> [Accessed 05 April 2018]
- Holley, J., Akhundov, O., Nolte, E., MacLehose, L., McKee, M. (2004). Health Care Systems in Transition. Azerbaijan. Health Care Systems in Transition, 6(8), pp. 1–76.
- Hovhannisyan, S.G., Tragakes, E., Lessof, S., Aslanian, H., Mkrtchyan, A. (2001). Health Care Systems in Transition. Armenia. Health Care Systems in Transition, 3(11), pp. 1–81.
- Ibrahimov, F., Ibrahimova, A., Kehler, J., Richardson, E. (2010). Azerbaijan. Health System Review. Health Systems in Transition, 12(3), pp. 1–115.
- Joseph, G., da Silva, I.C.M., Wehrmeister, F.C., Barros, A.J.D., Victora, C.G. (2016). Inequalities in the coverage of place of delivery and skilled birth attendance. Analyses of cross-sectional surveys in 80 low and middle-income countries. Reproductive health, 13(77), pp. 1–13.
- Karanikolos, M., Kühlbrandt, C., Richardson, E. (2014). Chapter 5. Health workforce. In: B. Rechel, E. Richardson, M. McKee, ed., Trends in health systems in the former Soviet countries. United Kingdom: World Health Organization Observatory Studies Series, 35, pp. 77–90.
- Kollar, E. and Buyx, A. (2013). Ethics and policy of medical brain drain. A review. Swiss medical weekly, 143(w13845), pp. 1–8.
- Lahtinen, P., Leino-Kilpi, H., Salminen, L. (2014). Nursing education in the European higher education area Variations in implementation. Nurse Education Today, [online] 34, pp. 1040–1047. Available at: <https://www.nurseeducationtoday.com/article/S0260-6917(13)00352-3/pdf> [Accessed 28 April 2018]
- Lefèvre, C. and Hohmann, S. (2014). Post-Soviet Transformations of Health Systems in the South Caucasus. Central Asian Affairs, 1(1), pp. 48–70.
- Liu, J.X., Goryakin, Y., Maeda, A., Bruckner, T., Scheffler, R. (2016). Global Health Workforce Labor Market
Projections for 2030. World Bank Group Policy Research Working Paper, [online] 7790, pp. 1–38. Available online at: <http://documents.worldbank.org/curated/en/546161470834083341/Global-health-workforce-labor-marketprojections-for-2030> [Accessed 05 April 2018] - McPake, B., Maeda, A., Araújo, E. C., Lemiere, C., El Maghraby, A., Cometto, G. (2013). Why do health labour market forces matter? Bulletin of the World Health Organization, 91(11), pp. 841–846.
- Nair, M. and Webster, P. (2013). Health professionals’ migration in emerging market economies. patterns, causes and possible solutions. Journal of public health, 35(1), pp. 157–163.
- National Statistical Service of the Republic of Armenia and the World Bank (2017). Part 3. Armenia. Non-material poverty. [pdf] pp. 127–180. Available at: http://www.armstat.am/file/article/poverty_2017_english_4.pdf [Accessed 10 April 2018]
- News.am, (2017). Հայաստանում ներդրվել է բուժաշխատողների շարունակական մասնագիտական զարգացման (ՇՄԶ) կրեդիտային մոդելը (Continuing Professional Development (CDM) credit model introduced in Armenia). [online] Available at: <https://med.news.am/arm/news/14324/hayastanum-nerdrvel-e-buzhashkhatoxneri-sharunakakanmasnagitakan-zargacman-shmz-kreditayin-modely.html> [Accessed 10 April 2018]
- Petrosyan, V., Melkomian, D.M., Zoidze, A., Shroff, Z.C. (2017). National Scale-Up of Results-Based Financing in Primary Health Care. The Case of Armenia. Health Systems and Reform, 3(2), pp. 117–128.
- Richardson, Erica (2013): Armenia. Health System Review. Health Systems in Transition, 15(4), pp. 1–99.
- Rzayeva, S. (2013). Oil and Health Care in Post-Soviet Azerbaijan. European Journal of Sociology, 54(01), pp. 33–63.
- The Ministry of Education Republic of Azerbaijan (2009). State program on reforms in the higher education system of the Republic of Azerbaijan for the 2009–2013 years. [online] Available at: <http://edu.gov.az/en/page/299/2553>
- The National Statistics Office of Georgia, 2018. [online] Available at: <http://www.geostat.ge/index.php?action=page&p_id=1145&lang=eng> [Accessed 17 April 2018]
- The State Statistical Committee of the Republic of Azerbaijan, 2018. [online] Available at: <https://www.stat.gov.az/?lang=en> [Accessed 17 April 2018]
- The Statistical Committee of the Republic of Armenia, 2018. [online] Available at: <http://www.armstat.am/am/?nid=130> [Accessed 17 April 2018]
- The World Health Organization (2016). Global strategy on human resources for health: Workforce 2030. [pdf] pp. 1–61. Available at: <http://apps.who.int/iris/bitstream/handle/10665/250368/9789241511131-eng.pdf;jsessionid=46471682592DBAC10EC0137E9805FE47?sequence=1> [Accessed 05 May 2018]
- The World Health Organization (2016a). Health workforce requirements for universal health coverage and the sustainable development goals. Human Resources for Health Observer Series, [online] 17(1), pp. 1–34. Available at: <http://apps.who.int/iris/bitstream/handle/10665/250330/9789241511407-eng.pdf?sequence=1> [Accessed 28 April 2018]
- The World Health Organization Regional Office for Europe, 2010. Rural poverty and health systems in the WHO European Region. [pdf] pp. 1–34. Available at: <http://www.euro.who.int/__data/assets/pdf_file/0019/130726/e94659.pdf> [Accessed 10 April 2018]
- The World Health Organization, 2010. WHO Global Code of Practice on the International Recruitment of Health Personnel. [pdf] pp. 1–12. Available at: <http://www.who.int/hrh/migration/code/code_en.pdf?ua=1>
The World Health Organization, 2016. Global Health Observatory data repository. [online] Available at: <http://apps.who.int/gho/data/node.main> [Accessed 17 April 2018]
About the Author
Gulnaz Isabekova is a researcher of the CRC 1342 “Global Dynamics of Social Policy” based at the Research Centre for East European Studies at the University of Bremen.
Healthcare Workers in Armenia, Azerbaijan and Georgia
Density of Health Care Personnel
Table 1:1: Density of Physicians, Nurses and Midwives per 1,000 Population
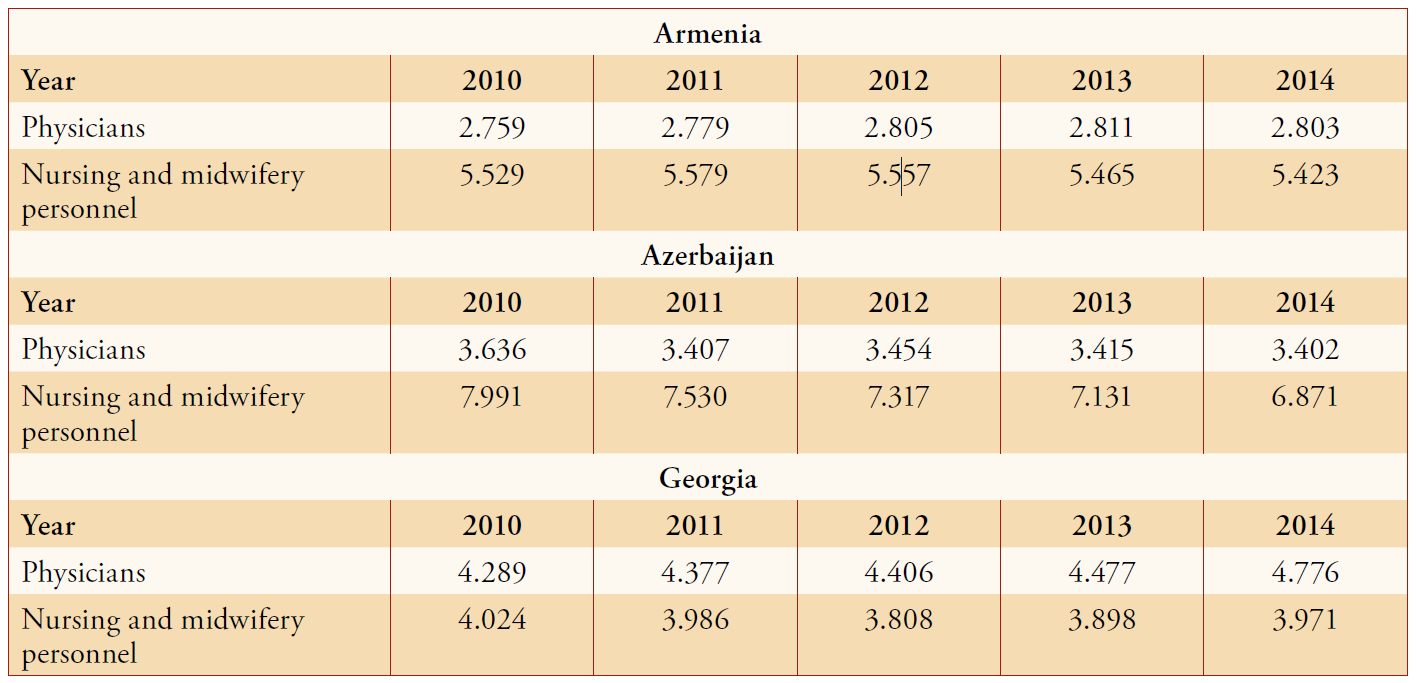
Table 1.2: Average Density of Physicians, Nurses and Midwives per 1,000 Population (2010–2014)
Distribution of Healthcare Workers by Specialties
Table 2.1: Absolute Number of Physicians, Nurses and Midwives
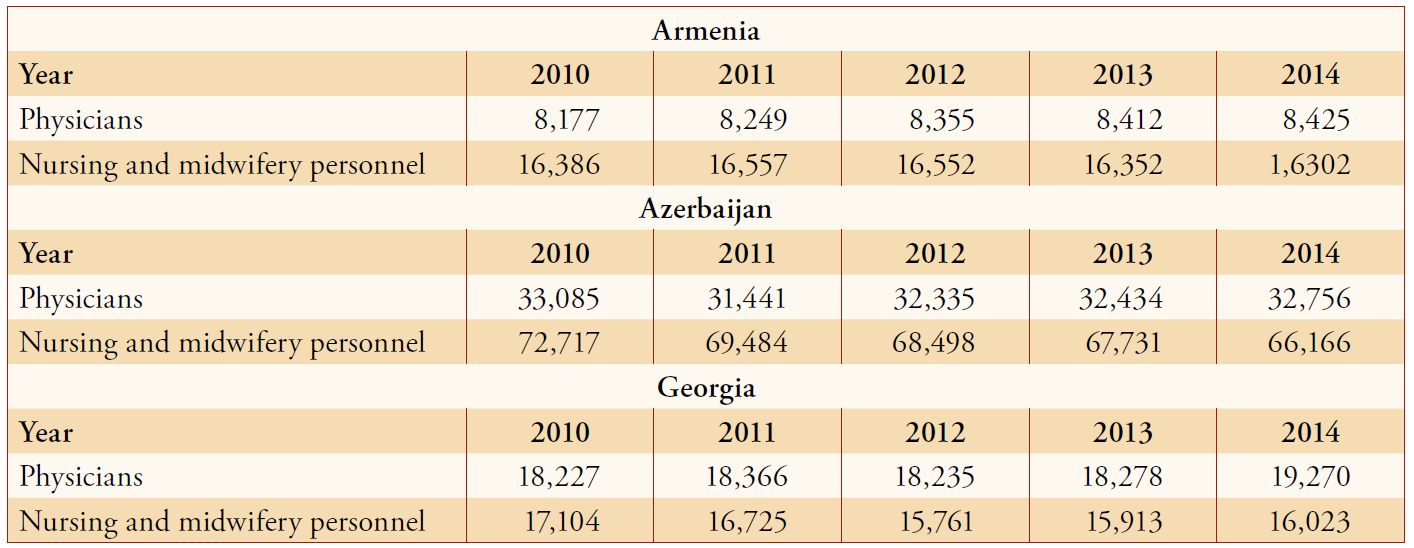
Table 2.2: Disaggregated Data on Nurses and Midwives
Regional Distribution of Healthcare Workers1
Table 3.1: Number of Doctors per 10,000 Population in Armenia
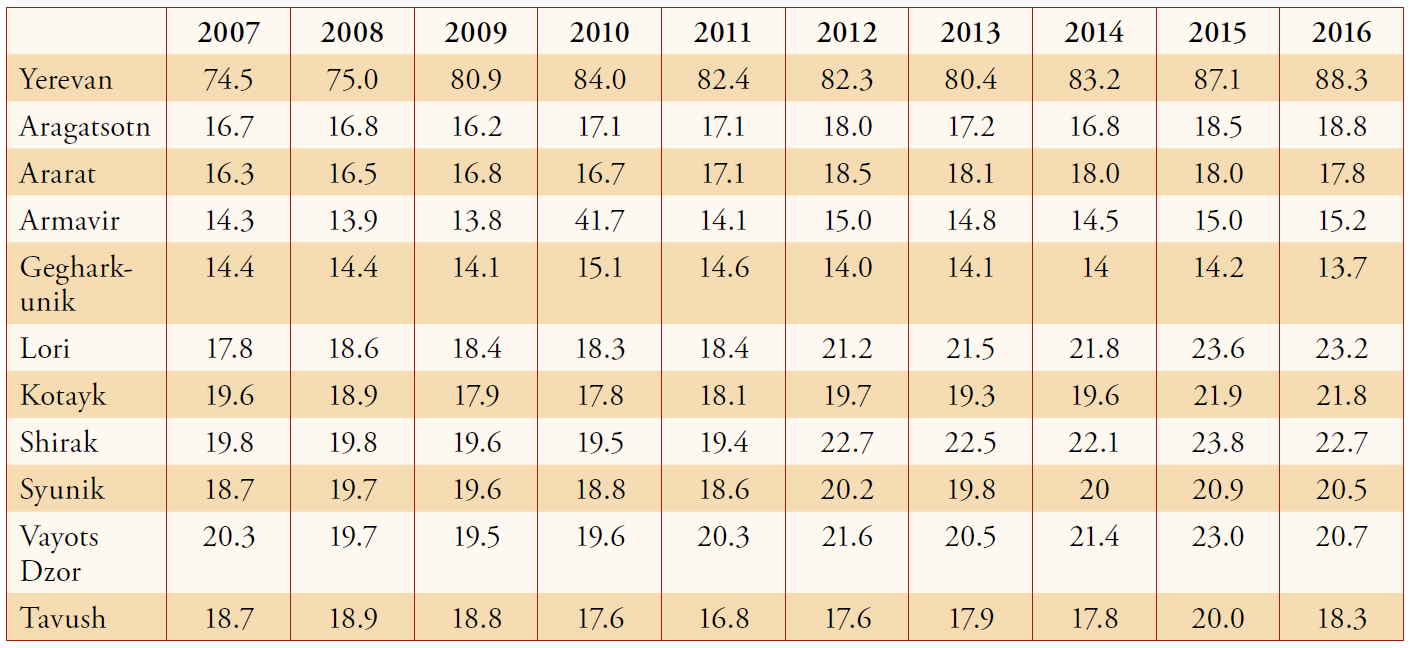
Table 3.2: Mid-Level Healthcare Workers per 10,000 Population in Armenia
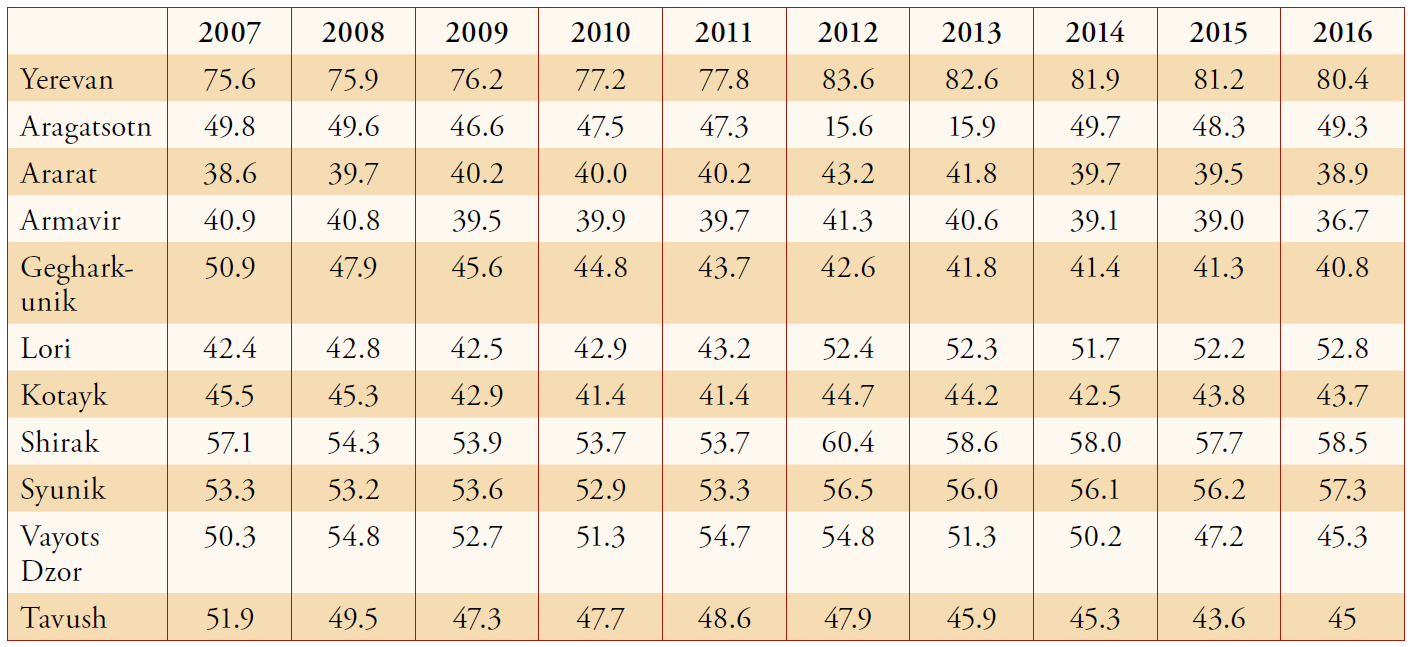
Table 3.3: Doctors per 10,000 Population in Azerbaijan
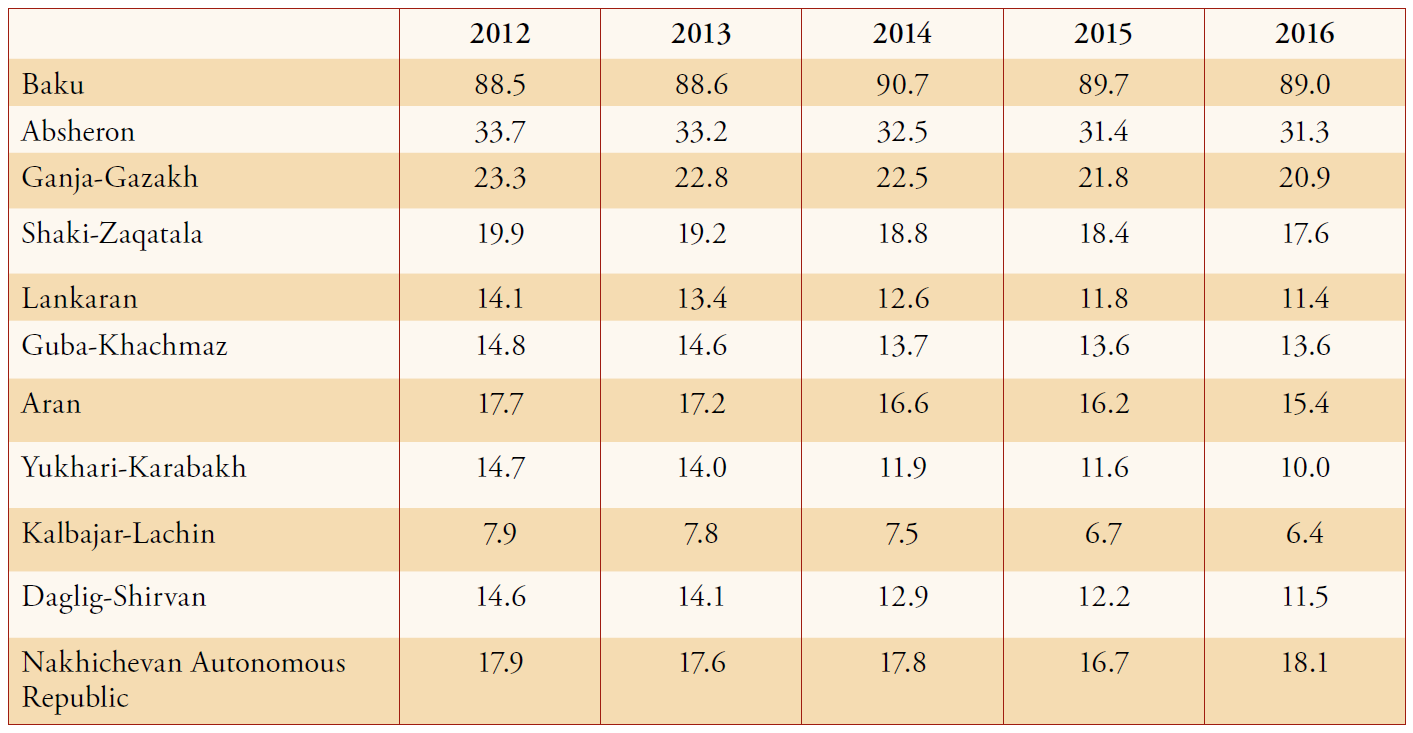
Table 3.4: Mid-Level Healthcare Workers per 10,000 Population in Azerbaijan
Health Expenditures
Table 4.1: Current Health Expenditure (as Share of GDP): Post-Soviet Region
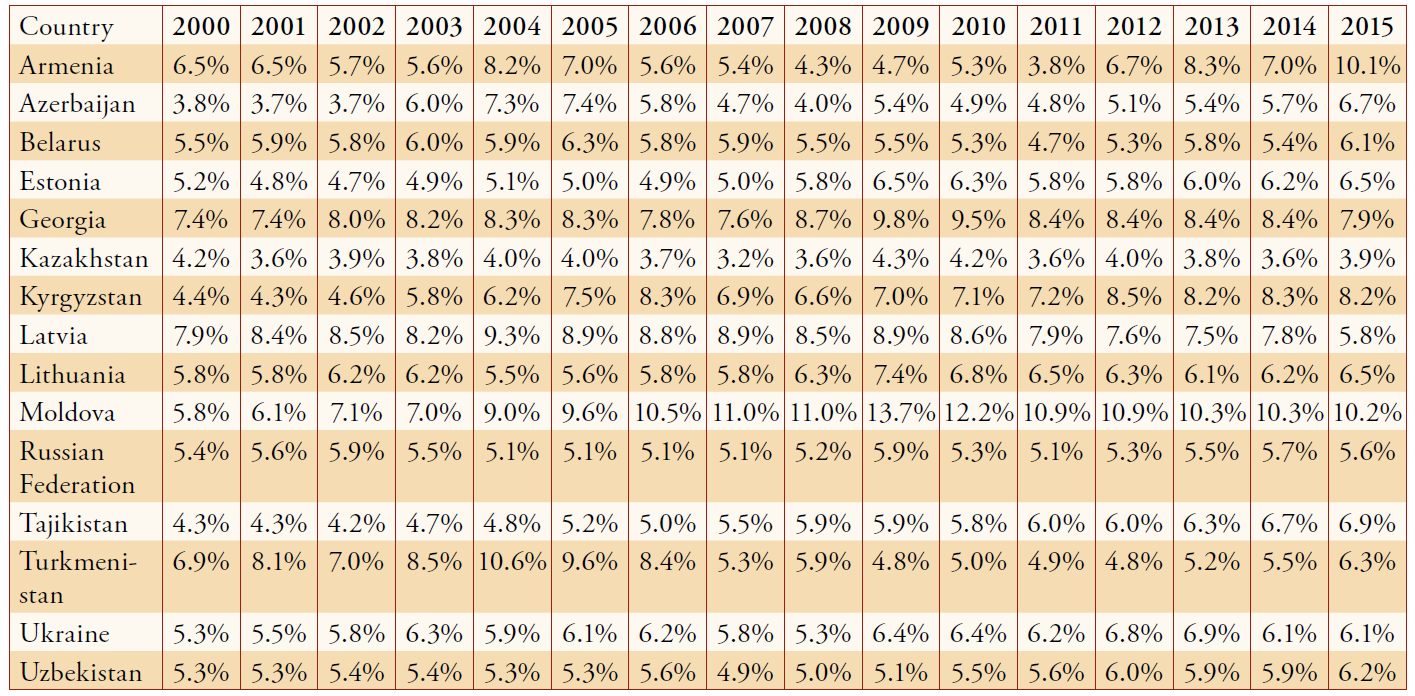
Table 4.2: Domestic General Government Health Expenditure as Percentage of Current Health Expenditure (%)
Healthcare Workers’ Salaries
Table 5.1: Monthly Nominal Wages in Armenia in Armenian Dram (AMD)2
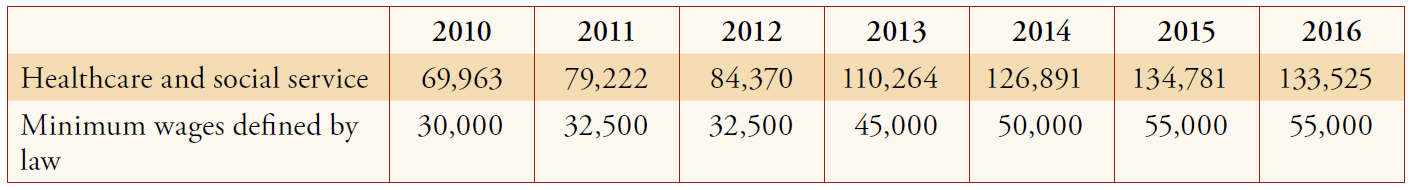
Table 5.2: Monthly Nominal Wages in Azerbaijani Manat (AZN)
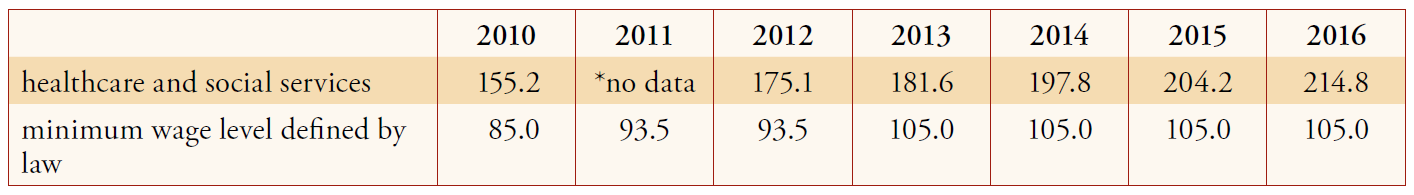
Table 5.3: Monthly nominal wages in Georgian Lari (GEL)3
Notes
1 Data on regional distribution of healthcare professionals is not available on the website of the National Statistics Office of Georgia, which contains general data on the number of physicians etc. but not their distribution <http://www.geostat.ge/index.php?action=page&p_id=197&lang=eng>. For this reason there is no table on Georgia.
2 Since 2011 there is a distinction between public and private employees’ average earnings. I took numbers for the public workers.
3 The data on minimum wages could not be found, therefore it was substituted by average nominal income.
For more information on issues and events that shape our world, please visit the CSS Blog Network or browse our Digital Library.

